NOTES ON THERAPY
From bite-sized insights to deep dives on healing, NOTES ON THERAPY is where mind meets meaning.
As therapists, staying informed about mental health is essential. Sharing current research and raising awareness helps to reduce stigma and makes mental health support more accessible and relatable in everyday life. Check out the blog posts below for the latest in psychology and mental health.
Rethinking Addiction
WHY IT’S NOT ABOUT MORALITY
When we reduce addiction to a question of right or wrong, we miss the pain, the history, and the human beneath it. Here’s why morality can’t explain addiction and what can.
Why It’s Not About Morality
When we reduce addiction to a question of right or wrong, we miss the pain, the history, and the human beneath it. Here’s why morality can’t explain addiction and what can.
Written by Emma Nagle, LCSW } November 10, 2025
Addiction is not a “moral failing” or a reflection of weak character.
It is a complex and multifaceted response to pain, stress, and trauma. Many people who develop substance use disorders are attempting to manage overwhelming emotional states, intrusive memories, or chronic distress that feel intolerable without external relief.
Substances temporarily alter the nervous system, dampening hyperarousal responses, numbing painful emotions, or filling the void created by disconnection and loss.
Over time, these coping mechanisms, though initially adaptive in their intent to reduce suffering, become maladaptive and self-perpetuating as the person increasingly relies on substances to regulate mood and function.
Repeated substance use fundamentally changes brain chemistry, particularly within the reward, motivation, and stress regulation systems. The brain begins to associate substance use with survival, reinforcing cravings and compulsive behaviors even when the individual intellectually understands the harm. This neurobiological conditioning can override logic and willpower, creating a cycle of craving, use, and shame that deepens the sense of helplessness.
By understanding the driving forces and the science behind addiction, treatment can become more integrative. This means programs and providers can address co-occurring mental health conditions simultaneously with therapy and psychotropic medication when necessary. Additionally, treatment can become more individualized. Providers can reach the person suffering by beginning to understand the experiences that led to self-medicating. Treating addiction from the viewpoint of moral failing sends the message to a person addicted that they are of weak character or lack of willpower. This type of messaging can risk causing further shame and emotional pain that perpetuates the cycle of using.
Understanding addiction through a biopsychosocial lens rather than through one of morality, allows for compassion, accountability, and effective treatment that targets the underlying trauma and emotional pain driving the behavior. If you are struggling with substance use or know someone who is, consider: What is this drug treating? This might give you the key to the next step in unlocking how to recover from the cycle of addiction.
If you or a loved one are struggling with addiction, help is available. You can book a consultation call with me here, to see if individual therapy is right for you, or find help and support near you on SAMHSA’s website.
What is recovery dharma?
Recovery Dharma offers an alternative to AA by using Buddhist principles like mindfulness and compassion to support addiction recovery. Learn how this community takes a different path toward healing and self-awareness.
Recovery Dharma applies Buddhist principles directly to addiction recovery.
Written by Emma Nagle, LCSW | September, 29, 2025
For nearly a century, Alcoholics Anonymous and its 12-step philosophy have dominated the landscape of addiction recovery. Its influence is so widespread that for many, it’s the only social support model they’ve ever been offered. But as conversations around mental health, trauma, spirituality and neurodiversity deepen, so too does a growing recognition that recovery isn’t one-size-fits-all. Out of disillusionment and growing awareness of just how diverse the population affected by addiction truly is, alternative secular mutual support organizations like SMART Recovery, which focuses on Cognitive-Behavioral Therapy based skills and in the 2010’s, Refuge Recovery, a Buddhist-based community, began to develop. What follows is an exploration of Recovery Dharma — how Buddhist teachings on suffering, impermanence, and compassion can offer a radically different approach to healing. We’ll consider how it stands alongside traditions like AA, while carving out its own space for those seeking a path less tethered to faith. Along the way, you’ll find glimpses of what meetings feel like and where to turn if you sense this might be a community for you.
Buddhism offers a more flexible pathway to spiritual healing that does not involve “defects of character,” and instead proposes that: Suffering is part of life, but through awareness, ethical living, and mindful presence, we can reduce suffering and cultivate freedom. At its core, Buddhism teaches that craving, attachment, and aversion are the roots of suffering and that liberation comes from seeing these clearly, responding with compassion, and living with intention. This concept of suffering resonates for many stuck in the cycle of addiction and has since become a fully-formed addiction recovery program with a growing community.
Before discussing the Buddhist-based approach to recovery in detail, it is important to note the rupture that occurred within Refuge Recovery in 2018 following allegations made against the founder of the program Noah Levine, that led to a significant portion of the community breaking away and intentionally forming a separate leaderless, peer-governed organization. This new non-hierarchical organization was designed to be non-charismatic and rooted in shared wisdom rather than individual authority and became known as Recovery Dharma.
So, What is Recovery Dharma?
Recovery Dharma is a peer-led movement and community that is founded on the trust in the potential for all to recover and find freedom from the suffering of addiction. Recovery Dharma offers a path to healing that blends ancient Buddhist principles with the lived experience of addiction recovery.
In this community, Buddhist teachings, known as the Dharma, are applied to addiction recovery in an effort to live a life of true freedom and emphasizes personal agency and empowerment over powerlessness seen in the 12-step approach. Recovery Dharma sees addiction as a form of suffering rooted in craving and disconnection. The practices and principles used are applicable for all types of addictions (alcohol, drugs, process addictions) and really any repetitive or habitual behavior that is causing suffering.
The path to healing involves mindfulness, self-inquiry, and community support, not shame, willpower or moral judgment. A commitment to abstinence or thoughtful boundaries* with the behavior are asked for to allow for awareness of the relationship to the behavior and any other harmful behaviors to become apparent. The Recovery Dharma (2023) book states, “Recovery is a lifelong, holistic process of peeling back layers of habits and conditioned behaviors to find our own potential for awakening.” While on the path to healing expect to commit to deepening your understanding of the Four Noble Truths and to practicing the Eightfold Path (the core texts that guide the community in RD) in daily life.
*Thoughtful boundaries may be required when abstinence is not possible or probable such as in the case with food and sex addiction.
The belief is that through practices like meditation, honest reflection, and ethical living, people can learn to face discomfort rather than escape it. Recovery Dharma describes this as a philosophy and a plan of action - all found in the Eightfold Path. The investigation of one’s mind through a meditation practice is a major component of the work and encouraged to be practice in and outside of meetings. Below you’ll find an introduction to the teachings that are the foundation of the program.
“Recovery is rooted in finding our own
inner wisdom & individual journeys.”
The Four noble truths
The Four Noble Truths, lessons from the Buddha about the cycle of existence, are at the heart of the Dharma.
These four truths below, and the corresponding commitments, are the foundation of the Recovery Dharma program:
There is suffering.
We commit to understanding the truth of suffering.
There is a cause of suffering.
We commit to understanding that craving leads to suffering.
There is a way of ending suffering.
We commit to understanding and experiencing that less craving leads to less suffering.
There is a path that leads to ending suffering.
We commit to cultivating the path.
Similar to “working the steps” in Alcoholics Anonymous, The Four Noble Truths in Recovery Dharma are explored through writing and sharing in-depth, detailed inquiries found in the book. These can be worked on with the guidance of a mentor or therapist, in partnership with a trusted friend, or with a peer group. An Inquiry Circle are small closed groups who meet weekly with the goal of completing their inventories. The fourth noble truth tells us that there is a way to end suffering by following the Eightfold Path, listed below:
THE Eightfold path
Wise Understanding
Wise Intention
Wise Speech
Wise Action
Wise Livelihood
Wise Effort
Wise Mindfulness
Wise Concentration
The Eightfold Path is a way of life that is followed and practiced to the best of one’s understanding and capacity. In other words, how this practice will be interpreted is up to you. The Path can serve as both a religious and non-religious journey.
Rather than labeling people as “addicts,” and contrary to most well-known mutual support organizations available, Recovery Dharma emphasizes impermanence, non-identification, and the belief that everyone has the capacity to wake up and change. The Recovery Dharma text encourages the customization of one’s recovery course - a refreshing take on healing for many who have felt out of place in the framework of stricter programs.
Powerlessness is a key component of common recovery work, where personal weakness is highlighted, and reliance on external willpower and higher powers is valued. Recovery Dharma's view on powerlessness is nuanced: it's not about personal weakness, but about a profound understanding of craving and attachment as the root of suffering, as taught in Buddhist principles. By acknowledging this powerlessness over addiction's grip, individuals are encouraged to engage in the process of letting go of attachments, using mindfulness and meditation to develop inner strength and find freedom, rather than relying on external willpower or higher powers.
One of the aspects that makes Recovery Dharma distinct is that it does not require members to adopt Buddhist beliefs or any religious framework. While the program draws inspiration from Buddhist principles like mindfulness and compassion, participation is not tied to faith or doctrine. This stands in contrast to 12-step programs such as AA, where the language of “God” and prayer are woven into the structure of meetings. Even with the flexibility to interpret “God” more loosely like “Good Orderly Direction,” for example, many people find the faith-based tone and higher power concept to be alienating. Recovery Dharma offers a different path: one grounded in meditation, self-inquiry, and community support, without the need for prayer or spiritual hierarchy.
What to Expect at a Recovery Dharma Meeting
A typical Recovery Dharma meeting begins with a guided meditation (15-20 minutes), followed by a reading from the Recovery Dharma text, and then group discussion or sharing. Participants reflect on how the reading or meditation connects to their own recovery, though speaking is always optional. Listening is equally valued. Meetings are peer-led, welcoming, and emphasize confidentiality. Like most mutual support meetings, formats vary (book study, open sharing, or meditation-focused), but all offer a supportive space to practice mindfulness, explore cravings and emotions, and connect with others on a similar path. The meeting ends with a closing reading or ritual, often a “Dedication of Merit.” This is a way to conclude together, expressing goodwill or positive intention. RD offers meetings (sangha groups) online and in-person, however the abundance of meetings in your area may be limited due to the fact that the community is still growing in popularity.
“Recovery means empowerment and we support
each other as partners walking the path together.”
Expanding the Path
Recovery Dharma has grown because so many people struggled to feel at home in traditional mutual support groups. For those who did not connect with prayer, faith-based language, or the idea of surrendering to a higher power, the path forward often felt limited. Out of this need came a community that centers mindfulness, compassion, and personal responsibility. The rise of Recovery Dharma is a reminder that there is no single blueprint for recovery. People need different kinds of spaces to heal, and for many, meditation and Buddhist-inspired practices offer a grounding, non-dogmatic alternative. At its best, Recovery Dharma is not just a program, but a movement. One that expands the landscape of recovery so more people can find a place where they truly belong.
Recovery Dharma reminds us that healing can be both personal and communal. That recovery is not about adhering to a rigid framework, but about finding practices that allow for curiosity, connection, and self-compassion. Whether through meditation, shared wisdom, or the supportive presence of others on the same path, this approach provides space for those who seek recovery without the overlay of religious language or belief systems. At its heart, Recovery Dharma offers not just freedom from addiction, but the possibility of living with greater clarity, balance, and meaning.
NO MUD,
no lotus.
Want to Learn More?
Read the Recovery Dharma book here.
Find a meeting here.
Listen to meditation audio recordings or read meditation scripts here.
Need a different kind of addiction support? Call 1-877-8-HOPENY (467369)
Have a loved one struggling with substance use? Check out this article: How To Support a Loved One With Addiction.
Why Risk Becomes Irresistible
The Psychology of Gambling Addiction
The Psychology of Gambling Addiction
Written by Emma Nagle, LCSW | September 20, 2025
Behind the bet lies more than chance.
Gambling addiction is a complex mix of psychology, reward systems, culture and emotional needs. This article explores why and how gambling can become addictive, what keeps people hooked, and the paths toward recovery.
When most people think of gambling addiction (also known as a gambling disorder in the DSM-5 or compulsive gambling), they imagine someone chasing money or the thrill of winning. But the truth is, gambling problems usually go much deeper than that. Gambling affects the brain’s reward system, taps into powerful emotions, and often hides underlying struggles. Understanding these layers can help explain why it’s so hard to stop, how our culture can perpetuate behavior and how recovery is possible.
By definition, a Gambling Disorder is persistent and recurrent problematic gambling behavior leading to clinically significant impairment or distress. This is indicated by four or more of the following in a 12-month period:
1..Needs to gamble with increasing amounts of money in order to achieve the desired excitement.
2. Is restless or irritable when attempting to cut down or stop gambling.
3. Has made repeated unsuccessful efforts to control, cut back, or stop gambling.
4. Is often preoccupied with gambling (e.g., having persistent thoughts of reliving past gambling experiences, handicapping or planning the next venture, thinking of ways to get money with which to gamble).
5. Often gambles when feeling distressed (e.g., helpless, guilty, anxious, depressed).
6. After losing money gambling, often returns another day to get even (“chasing” one’s losses).
7. Lies to conceal the extent of involvement with gambling.
8. Has jeopardized or lost a significant relationship, job, or educational or career opportunity because of gambling.
9. Relies on others to provide money to relieve desperate financial situations caused by gambling.
Why Do People Get Addicted to Gambling?
Most gambling begins as a harmless, social activity. But over time, it can shift into something more consuming and signs of impairment such as the symptoms listed above begin to appear and affect daily life. Triggers to the brain’s reward system causing cravings and impaired inhibition, maladaptive coping strategies, genetic vulnerabilities, targeted marketing, and the very design of chance-based games all play a role in why gambling becomes addictive.
The Brain’s Reward System
At its core, gambling is designed to keep people hooked. The highs and lows trigger brain chemistry in a way that makes walking away incredibly difficult. The concept of addictive games and social media platforms has become well-known in recent years due to the rise of mobile games like Candy Crush and apps like TikTok. What makes these platforms addictive is also what fuels gambling: dopamine spikes tied to unpredictable rewards.
Dopamine highs:
Every win and even near misses that feel like you almost won floods the brain with dopamine, the same “feel good” chemical involved in drug use. This makes gambling exciting and addictive, just like other drugs. With constant dopamine release over time, the brain’s pleasure and motivation system (known as the limbic system) can become hijacked, leading to an imbalance that weakens the brain's natural braking mechanisms for controlling impulses.
Unpredictable rewards:
Slot machines, poker, and sports betting all rely on chance. Because the reward is unpredictable, the brain keeps pushing for “just one more try.” Psychologists call this a variable ratio reinforcement schedule, and it’s one of the most powerful conditioning tools there is.
Every time someone places a bet, the brain anticipates a payoff. Even when there isn’t a win, the possibility of one releases dopamine. This variable reward schedule, never knowing when the “big win” will hit, keeps people coming back, much like pulling a slot machine lever again and again. Over time, the brain starts craving not just the win, but the rush of anticipation itself.
Emotional Needs and Psychological Drivers
Beyond brain chemistry, gambling often serves as a way to cope with difficult feelings. For many people, it becomes less about winning money and more about managing emotions. Gambling may be a way to avoid painful memories, fill an emotional void, or cope with stressors that feel overwhelming. A gambling disorder can also co-occur with substance use disorders, mood disorders and other mental health issues. Below are some of the most well-studied motivators for gambling behavior.
Escape from pain: Gambling can temporarily numb stress, depression, anxiety, or grief. Sometimes it can even lead to feelings of pleasure due to the neurotransmitter dopamine. As gambling behaviors begin to have a negative impact one’s life, stressors may exacerbate feelings of depression and anxiety causing a need for further escape that becomes cyclical and isolating.
Illusion of control: Many gamblers believe their rituals, strategies, or intuition affect outcomes. Cognitive distortions like ‘near misses’ and ‘hot streaks’ create a false sense of control (and hope) that keeps them engaged. A sense of control can feel extra rewarding if someone is feeling particularly out of control in other areas of their life.
On the flip side of this, strong core beliefs of helplessness, or in periods of depression, anxiety and desperation, can result in too much emphasis on luck such as, “My life will only change if I get lucky.”
Chasing losses: After losing, the urge to keep playing in hopes of “getting it back” can feel irresistible. This is considered to be a hallmark of the transition from recreational to disordered gambling. Each new bet can feel like a chance to undo past mistakes, but instead it deepens the cycle of desperation and shame. What begins as an attempt at repair often ends up creating even greater financial and emotional damage.
Boost to self-esteem: Wins provide a short-lived sense of confidence and value, but losses often reinforce shame creating a painful cycle. As a therapist, it is important to assess what kind of meaning and significance financial security or success might hold for someone. For many, money isn’t just about paying bills, it represents safety, belonging, or even proof of being “good enough.” Gambling taps into these hidden assumptions, where financial wins are equated with self-worth and losses confirm deep fears of inadequacy or failure.
This dynamic can drive insecurity, especially when early experiences or cultural messages have tied personal value to achievement or material success. When someone carries distorted beliefs such as “I’m only lovable if I succeed” or “Without money, I’m nothing,” gambling can become a powerful but destructive way to test or repair those internal narratives.
The Role of Society and Technology
It’s not only internal psychology that fuels gambling. We all know some of the tactics casinos use to keep players engaged for hours at a time: using chips instead of physical money, not having clocks or windows in casinos, free drinks etc. External forces like betting apps, advertising, and social norms continue to make it harder to step away. Modern gambling is designed to be fast, accessible, and always within reach.
The digitization and commercialization of sports betting apps increases visibility and accessibility.
FanDuel and DraftKings have become popular with the rise in live sports betting and offer seamless transactions. Online casinos are available 24/7, which feeds into the brain’s difficulty with impulse control. They also allow for players to engage in multiple games at once, keeping a player engaged despite potential losses. Newer platforms like Polymarket, better described as a prediction market, is further expanding what a bettor is capable of from their phone or computer. Betting is no longer limited to games and sports, but has grown to include, politics, economics, news, culture and more. This platform draws users in by way of cryptocurrency.
There has been a significant societal shift. What was once seen as a fringe activity, has now become mainstream. Marketing normalizes gambling as fun, social, and even glamorous. Sports sponsorship by gambling companies plays an important role in normalizing gambling within communities.
Algorithms encourage continued play by tracking behavior and tailoring promotions. Widespread and often unregulated gambling advertising can expose and target vulnerable individuals and even children, potentially leading to increased gambling problems later in life. Advertising can be deceptive, especially for new bettors when suggesting it is “risk-free.” Online casinos use features like celebratory lights and sounds, which stimulates the brain's reward system and makes players feel like they are winning, even when they are losing money.
Recent Policy and Legal Updates in New York State
In recent years, gambling in New York has expanded rapidly, especially with the legalization of mobile sports betting and the growth of online platforms. These changes have made gambling more accessible than ever, which can increase both recreational play and the risk of addiction. Staying informed about shifts in policy helps highlight how the landscape is evolving and why support and awareness are more important than ever.
Here are a few important details about changes that are intended to increase consumer protections, reduce harmful emergent behaviors, and regulate how sports betting and gambling are accessed and promoted especially via mobile apps.
Online/mobile sports betting legalization has been in effect since January 2022. Users must be physically located in NY to place mobile sports bets.
Proposed legislation (Bill A7962) would place limits on sports betting including daily or period deposit caps, advertising restrictions, and bans on using credit cards for mobile sportsbook deposits.
Actions taken against “sweepstakes casinos” (online platforms using virtual coins that can be redeemed for cash/prizes) have been shut down via cease-and-desist orders by the NY Attorney General. These violate state law that prohibits gambling involving “something of value” without oversight.
In October 2024, legislation signed by Govenor Hochul requires gambling and sports betting advertisements to include warnings about harmful and addictive effects and problem gambling hotlines.
As gambling becomes more accessible via technology (apps, sweepstakes-style games, etc.), these policies are relevant to anyone working in addiction recovery or mental health.
Treating Gambling Disorders
While gambling addiction can feel overwhelming, recovery is possible with the right supports in place. Treatment focuses not only on reducing harmful behaviors, but also on addressing the emotional, financial, and social challenges that keep the cycle going. Below are some of the key areas that can guide the recovery process.
Assessment and Awareness
For the person stuck in a cycle of compulsive behavior, the first step might be recognizing the extent of their gambling and how it impacts finances, relationships, and emotional health. Honest tracking of time and money spent can create a clearer picture of the problem. Speaking with a therapist or getting screened/assessed by an addiction counselor can help determine needs and next steps with privacy and without judgment.
Developing Coping Strategies
Since gambling often serves as an escape from stress or difficult emotions, treatment focuses on building healthier alternatives. This can include relaxation skills, urge surfing, structured daily routines, and new hobbies that provide reward without harm. Resetting dopamine by engaging in natural activities that boost mood can be helpful to incorporate. Collaboration with a professional around relapse prevention techniques may be key for identifying and avoiding triggers.
Addressing Underlying Issues
Many people gamble to soothe deeper feelings of anxiety, depression, grief, or low self-esteem. Therapy helps uncover these emotional drivers and create space for healing so gambling isn’t the only outlet. Feelings of gulit and shame take time to address in talk therapy. When mood disorders are present, the addition of psychiatry can help relieve symptoms more quickly through the use of psychotropic medications. Addressing substance use disorders is also imperative in ensuring abstinence to gambling behavior as one behavior tends to trigger the other. Setting small and obtainable goals and objectives for oneself can improve low self-esteem and reinforce progression in treatment.
Financial and Practical Supports
Putting safeguards in place is essential. This might involve limiting access to credit, enlisting a trusted support person to manage finances, or using tools to block gambling apps and websites. Transparency can be a helpful tool when involving a loved one as it reinforces accountability and rebuilds trust.
Community and Accountability
Recovery is often strengthened through support groups such as Gamblers Anonymous, Recovery Dharma, or other peer support networks. Having others who understand the struggle reduces shame and provides encouragement and guidance. Some find great support from the structure of the 12-step philosophy in GA, the abundance of meetings and from sponsorship.
Relapse Prevention
In greater detail, relapse prevention is essential and more than coping strageties. Since urges to gamble can resurface, therapy helps clients anticipate triggers, practice refusal skills, and prepare a plan for moments of high risk. Building a lifestyle with meaningful connections and activities also decreases vulnerability to relapse.
If you or someone you care about is struggling with compulsive gambling, problem gambling, or gambling disorder, you don’t have to face it alone. Healing is possible.
Helpful steps include:
Reach out for an evaluation from a licensed therapist who has experience with gambling addiction (book a consultation with me here).
Call 1-800-GAMBLER/Text 800GAM/Chat online
Explore peer support (Gamblers Anonymous), where you can talk with people who understand.
If you're ready, I offer telehealth sessions for those seeking recovery and deeper understanding. I can support you in finding tools to reduce harm now, while also working toward lasting change. Book a consultation with me here.
Unsure where you stand with your gambling behaviors? Take this questionnaire to learn more.
What ‘The Pitt’ Got Right About Addicted Medical Professionals
Written by Emma Nagle, LCSW | May 21, 2025
The character of confident, playful, senior resident Dr. Langdon in HBO Max’s The Pitt, offers a rare, honest glimpse into the hidden struggles of medical professionals dealing with addiction.
While fictional, Dr. Langdon’s story reflects a reality that I’ve encountered many times in my work as an LCSW and Clinical Supervisor in an New York outpatient substance use and mental health treatment clinic.
Over the years (and particularly since the COVID-19 pandemic) I’ve seen a notable rise in professionals, especially those in healthcare, getting connected to treatment. As The Pitt demonstrates, doctors, nurses, and other licensed clinicians carry immense responsibility and are routinely exposed to trauma, high-stakes decision-making, and chronic sleep deprivation. The culture of medicine often demands stoicism and self-sacrifice, leaving little room to tend to one’s own mental health. The show also explores a less talked-about dynamic: the pride that comes from 'doing the most.' There is a sense of validation and identity that can form around being the one who saves lives or works the longest shift, no matter the personal cost. As Langdon describes it, he is connected to the identify of being one of “the bees protecting the hive.”
It’s no surprise that burnout, depression, and substance use disorders are common among this group. Yet, seeking help can be incredibly complicated. Medical professionals not only fear stigma, they fear career consequences. Many face mandatory reporting, disciplinary action including license revocation, or professional monitoring. In New York City’s public hospital systems, the pressure to keep functioning under high patient volumes, staffing shortages, and institutional strain only amplifies this tension, much like The Pitt exposes.
What The Pitt gets right is the complexity. Dr. Langdon isn’t portrayed as reckless or weak. He’s a skilled, committed, senior resident, and quietly unraveling under the weight of his work and unprocessed pain. It mirrors what I’ve seen in real life: professionals who are high-performing, deeply caring, and profoundly isolated in their suffering. In fact, The American Association of Nurse Anesthetists (AANA) reports that approximately 10% to 15% of all clinicians will misuse alcohol or other drugs during their careers. While support exists for these individuals, Caduceus meetings are not enough support and do not encompass all the different types of medical licensure out there and are reserved strictly for doctoral healthcare professionals.
It should be noted that the concept of staff members diverting medication is not unfamiliar.
The Pitt taught us how inconspicuous someone’s addiction can be, even for doctors in an emergency room environment where professionals have a trained eye. The discovery of Dr. Langdon’s diversion of benzodiazepines was an accurate depiction in that a colleague suspected him. Like many other professionals misusing substances, it required a colleague or supervisor reporting them for confrontation about their addiction to occur. The moment Dr. Langdon is cornered about his diversion of a controlled substance, he begins to unravel. He clearly fears not only for his job at Pittsburgh’s Trauma Medical Center, but for his license as a doctor that he has spent a minimum of eight years working towards.
What we don’t see in The Pitt series is what the attending, Dr. Robby, chooses to do with the knowledge that one of his supervisees is stealing medication and appears to be addicted to pills. We heard him threaten Dr. Langdon by reporting him, which leads to:
“30 day inpatient treatment program. Followed by random urine tests - 50-60 a year. Followed by mandatory NA meetings. Three to four times a week for the first three years… Of a five year program.”
This may sound excessive, but it is comparable to the types of consequences medical professionals might face and the process they go through. A medical professional who is caught on the job under the influence, diverting narcotics, or, chooses to surrender their license and seek help, will be connected to their respective Employee Assistance Program (EAP). The Committee for Physician Health (CPH), Professional Assistance Program (PAP) and Office of Professional Misconduct (OPMC) are just a few monitoring sources that become involved depending on the type of licensure.
Given the stigma that exists around addiction, plus the consequences of losing a job and temporarily a license, and five years of intense monitoring, medical professionals are not inclined to seek out help.
Despite awareness of and access to resources, concerns for confidentiality and the impact treatment might have on employment or other responsibilities hinders workers from seeking care before their substance use and mental health issues have progressed and become unmanageable.
The Pitt doesn't offer a full resolution to Dr. Langdon’s story, but perhaps there is more to revealed in Season 2. This show captures how the demanding work in the healthcare field and issues like chronic pain can cultivate addictions to medications. It highlights that addiction does not discriminate. It also exposes the difficult truth that addiction among medical professionals often goes unseen until a crisis forces it into the light. And even then, the path to recovery is long, complicated, and shadowed by professional risk.
In my own work, I’ve seen how deeply rooted the fear of losing one’s identity, license, or livelihood can be for healthcare workers struggling with substance use. The systems meant to protect patient safety often unintentionally deter providers from getting the help they need until their suffering becomes too visible to ignore.
My experience facilitating an “Impaired Professionals” group shed light on just how prevalent addiction and barriers to treatment, really are among professionals. This also includes those not in the healthcare field, such as lawyers and pilots who also risk losing licensure. For better or for worse, many of these professionals found their way to care because they were reported. As part of their healing process, therapy often includes looking at their relationship to their job and discovering their identity outside of their profession. Those that successfully make it back into practicing in the field are required to learn healthier boundaries in the workplace to be able to maintain recovery gains.
Ultimately, what The Pitt gets right are the intricacies of addiction in high-functioning professionals. It doesn’t sensationalize the downfall and thus far, doesn’t simplify the recovery. It shows us how the very qualities that make someone excellent at their job—drive, endurance, perfectionism—can also mask the symptoms of burnout and dependence. And while it leaves us wondering what will happen to Dr. Langdon, it offers an opening for an important conversation about how we, as providers, supervisors, and peers, can better support one another before the unraveling begins.
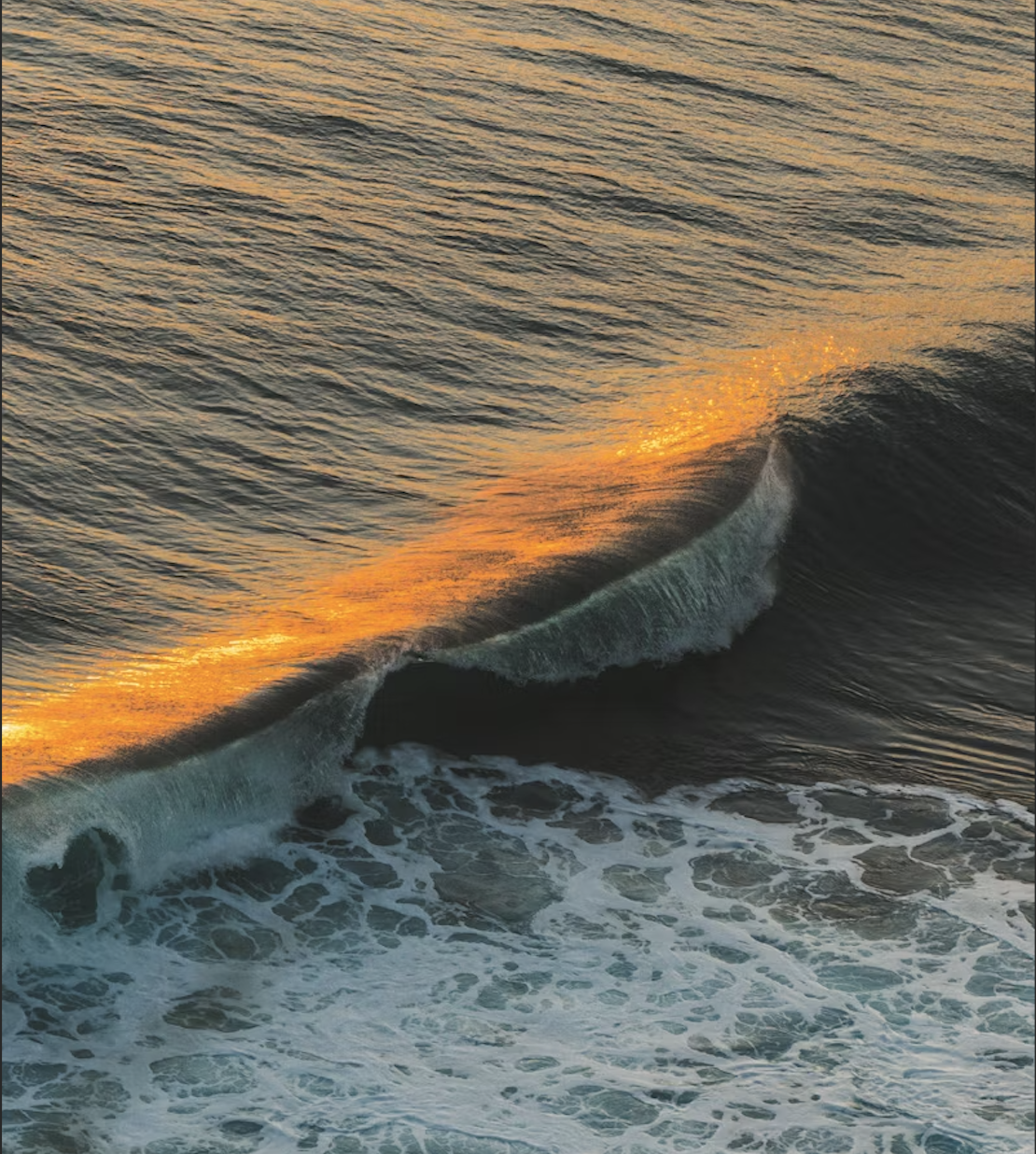
Surfing the Urge
Cravings and big emotions feel like overwhelming waves, but remember: you don’t have to drown in them. With urge surfing, you can ride through each swell, knowing it will pass. Just keep your balance, breathe, and trust the process. Read on to learn more about urge surfing.
Cravings and big emotions can feel like overwhelming waves, but remember: you don’t have to drown in them. With urge surfing, you can ride through each swell with awareness, knowing it will pass.
Ready to learn how to stay steady when the wave hits? Let’s dive in.
Written by Emma Nagle, LCSW | April 23, 2025
“I am not afraid of storms,
for I am learning how to sail my ship.”
-- Louisa May Alcott, Little Women
Urge surfing is a mindfulness technique that helps you manage unwanted behaviors by acknowledging and accepting urges without judging or acting on them.
Use the steps below as a guide to surfing the wave:
Identify the physical sensation of the urge
Visualize the urge as a wave that builds up, peaks, and then subsides
Observe the urge without fighting it
Ride out the urge until it passes...
Like real waves, urges rise and fall, they don’t last forever. The more you practice observing rather than reacting, the more your nervous system learns that you’re safe, even in discomfort. Urge surfing isn’t about willpower or resistance, it’s about building awareness, staying present, and trusting the temporary nature of emotional and physical impulses.
With time, urge surfing strengthens your ability to pause, reflect, and choose responses that align with your long-term values rather than short-term relief. For example, someone with an addiction might use this technique to sit with the discomfort of a drug craving; observing the urge without reacting or using, and instead, allowing it to pass. This practice not only helps prevent relapse, but also builds self-trust and reinforces the recovery process.
Each time you choose to ride the wave instead of reacting to it, you're practicing a new kind of resilience. Be patient and curious with yourself. Don’t judge your urges. Every urge you surf is a step toward greater self-regulation, freedom, and trust in your own inner stability.
How to Support a Loved One with Addiction
A CRAFT-Based Guide to Staying Connected Without Enabling
A CRAFT-Based Guide to Staying Connected Without Enabling
Written by Emma Nagle, LCSW | April 23, 2025
When someone you care about is struggling with substance use, it’s natural to feel helpless, scared, and unsure of what to do. You want to help, but you don’t want to enable. You want to set boundaries, but you don’t want to push them away. It’s a painful and confusing space to be in.
That’s where the CRAFT model comes in.
CRAFT stands for Community Reinforcement and Family Training. It’s a research-backed approach designed to help family members and close support systems learn how to effectively encourage a loved one toward treatment without ultimatums, guilt-tripping, or cutting them off.
As a therapist, I’ve seen CRAFT empower families and partners with tools that are not only compassionate and practical—but actually work.
Here’s a guide of how it works:
1. Understand What You’re Dealing With
CRAFT starts by educating loved ones on what addiction is: Not just a series of bad decisions, but a complicated behavioral pattern shaped by reward, habit, and pain systems in the brain.
Knowing this helps shift the mindset from:
“Why won’t they just stop?” to “What’s reinforcing this behavior, and how can we shift that?”
2. Notice What is Reinforcing the Substance Use
CRAFT teaches that people keep using substances because something about it “works” for them, whether it’s escaping stress, numbing pain, or just feeling normal for a moment. Their substance of choice should give insight into what they may be “treating” within themselves.
Your job isn’t to fix them, but to start recognizing how your responses might be (unintentionally) supporting the behavior.
Examples:
Are you giving money when they’re short because they spent it on substances?
Are you cleaning up their messes so they don’t face consequences?
This isn’t about blame. It’s about becoming more conscious of what’s keeping the cycle going.
3. Use Positive Reinforcement for Healthy Behavior
Here’s something refreshing: CRAFT isn’t about punishment. It’s about learning how to reinforce positive change, even in small doses.
Did they come home sober one night? Keep a therapy appointment? Go 24 hours without using?
Notice it.
Name it.
Appreciate it.
When you consistently reward healthier choices (with time, attention, calm conversation), you’re giving their brain a reason to keep trying.
4. Improve Communication Without Fighting
CRAFT encourages clear, kind, and assertive communication. That means less yelling, fewer power struggles, and no more walking on eggshells. Try using “I” statements and avoid blaming language.
Instead of saying:
“You’re ruining your life!”
You might try:
“I care about you, and I get scared when I see how much you’re using. I’d love to talk when you’re ready.”
This approach respects both your boundaries and their autonomy—two things that are crucial when trying to keep connection without enabling.
5. Support Treatment—But Let It Be Their Choice
A major goal of CRAFT is helping loved ones be more likely to accept help without being forced. CRAFT has been shown to be more effective than interventions that rely on confrontation or cutting people off.
You’re not trying to control their timeline. You’re helping create an environment where choosing help feels safe and supported. When they are ready to accept help, be ready to help. Have resources available or someone for your loved one to speak to further about their addiction.
final thoughts
Supporting someone through addiction is emotionally exhausting—but you don’t have to choose between doing everything and doing nothing.
CRAFT offers a third option: Stay connected. Set boundaries. Reinforce hope. All while taking care of yourself, too.
If you’re navigating this with someone you love, consider finding a therapist or support group to help ensure you are prioritizing your own emotional needs. Al Anon is one commonly sought out mutual aid resource for family and friends who have been affected by a loved one’s addiction. Support groups are a helpful reminder that you are not alone in this struggle. With the right tools, it is possible to make meaningful change—without losing your sanity, your compassion, or your connection.
Want a printable version of this guide? See below: